2025 BMES Annual Meeting Post Show Wrap-Up
Bridging Healthcare Gaps Through Biomedical Engineering The Biomedical Engineering Society (BMES) is excited to share the official 2025 Annual...
BMES serves as the lead society and professional home for biomedical engineers and bioengineers. BMES membership has grown to over 6,700 members, with more than 110+ BMES Student Chapters, three Special Interest Groups (SIGs), and four professional journals.
Welcome to the BMES Hub, a cutting-edge collaborative platform created to connect members, foster innovation, and facilitate conversations within the biomedical engineering community.
Discover all of the ways that you can boost your presence and ROI at the 2024 BMES Annual Meeting. Browse a range of on-site and digital promotional opportunities designed to suit any goal or budget that will provide maximum impact.
3 min read
Alan Brown 11/26/2024
This is two in a series of articles highlighting some of the technologies, processes and keynote plenary sessions presented at the 2024 Annual Meeting of the Biomedical Engineering Society, October 2024.
Extending Biomechanical Devices
The BMES Friday session, “Prosthetics, Biomechanics, and Assistive Technology” had the type of catchall name that promises a diverse range of subjects. It certainly delivered on that promise. Some of the most interesting papers ranged from neonatal respiratory models and heart assist devices to a faster, smoother way for exoskeletons to help disabled people walk.
Simulate neonatal respiratory systems. Researchers would like a cheap, inexpensive model to prototype respiratory monitors or practice imaging techniques without having to do animal testing. What they often get instead is a processed pig lung that costs about as much as a mid-sized car and is difficult to scale. For some, it also raises ethical issue. And such models simply do not exist for neonates and young children.
At Northwestern University, graduate student Heyang Wang faced that problem when his lab began looking for a better way to test its monitor prototypes. He decided to create an affordable, durable, anatomically accurate, and customizable (to simulate different medical conditions) model of a newborn’s lung, diaphragm, and thoracic cavity.
This proved more difficult than it sounds. Natural lungs have a complicated, branching hierarchical structure of passageways that deliver air deep into the lung. Lungs need to expand as they inhale as their artificial diaphragm compensates for the motion. And it needs to do this without high-pressure excursions during breathing.
To do this, Wang 3D printed the branching air passages from polylactic acid (PLA). He then cast a silicone elastomeric lung around it. After removing the lung, he washed away the PLA passageways with water. The result was a lung whose interior mimicked the hierarchy of a human lung.
Using flow and pressure monitors embedded in the lung, Wang was able to modulate the breathing rate and volume to emulate both neonates, children, and even adults. Compared with processed pig lungs, the elastomeric molding approach system provided the flexibility to adjust size, stiffness, and appearance to match different conditions. It also has the compliance needed for researchers to study obstructive lung diseases. Potential uses include wearable sensor validation, imaging system assessment, and medical training.
Keep dying hearts beating. For patients dying from heart failure, resuscitative thoracotomy is the final resort. It calls for surgeons to cut a patient’s chest open and literally keep the heart pumping by squeezing it with their hands. If the patient lives, they may implant an ECMO device, which bypasses the heart. This therapy is good for up to a few days. Other solutions include a hydraulic or pneumatic pump called a left ventricular assist device (LVAD) to move blood from the left ventricle into the aorta and through the body.
In both ECMO and LVAD systems, the mechanical pump comes in contact with blood. Because their surfaces are rigid, patients must take blood thinners to prevent cell damage and clotting. They are also dangerous to people aneurysms.
Another possibility is a mechanical actuator that applies pressure to the exterior of the left and right ventricles without coming in contact with blood, according to Kristoff Sarosi, a graduate student at ETH Zurich. Sarosi’s biventricular VAD (BiVAD) system consists of a controller to meter the force and speed of 3D-printed mechanical actuators placed directly on the heart. A vacuum pump keeps the devices securely attached to the epicardium.
Although the system might one day replace LVADs, the focus now is on finding a simpler alternative to pumping the heart by hand. Using an in vitro* sheep heart, the researchers compared their device with cardiac massage by an experienced surgeon. They demonstrated that the BiVAD could achieve a target cardiac output of 1.5 L/min, a level critical for patient survival. It was also more consistent, with fewer high-pressure peaks in both ventricles.
Sarosi’s team did notice some damage to the epicardium after three hours but noted that the system was a proof of concept with no padding on the actuators. Potential applications include treating ventricular fibrillation, myocardia infarction, cardiac arrest, and heart failure as well as organ preservation.
Control exoskeletons with kinematics. Children with cerebral palsy have excessive hip and knee floppiness and reduced knee extension. Exoskeleton can help them get around and strengthen their own muscles. One solution is a single-joint (knee) exoskeleton. These usually use a force-sensitive resistor located in the foot to track when the limb strikes the ground and when it lifts off again. An algorithm uses this data to regulate the force and torque applied to the exoskeleton.
This creates two issues, according to Jordan Dembsky, an Intramural Research Training Award (IRTA) postbaccalaureate fellow at the National Institutes of Health Clinical Center. First, it beats up sensors, which require frequent replacement. Second, the 150-millisecond gap between a foot strike and detection leads to an uneven gait.
This got Dembsky thinking about using estimated kinematics data from an inertial measurement unit to control gait, he would no longer need to measure foot strikes and send a lagged signal. A literature search found that for healthy individuals, the sagittal plane thigh angle maxed out at foot strike while hip joint angular velocity did the same for toe-off. Dembsky based his algorithm on detecting these peaks. This is especially difficult for children with cerebral palsy because of the irregular way they walk. This variation makes the data from the inertial measurement unit noisy. Dembsky compensated by using a high adaptive threshold, which analyzed each child’s individual gait and only recorded those over a certain magnitude.
The algorithm proved effective, capturing foot strikes within 40 milliseconds compared to 150 milliseconds for foot-based resistors. For toe-offs, it reacted within 85 milliseconds, at least on par with resistors. False positives and false negatives were each less than 1 percent, and the inertial measurement units proved more durable than the foot-based resistors.

Bridging Healthcare Gaps Through Biomedical Engineering The Biomedical Engineering Society (BMES) is excited to share the official 2025 Annual...
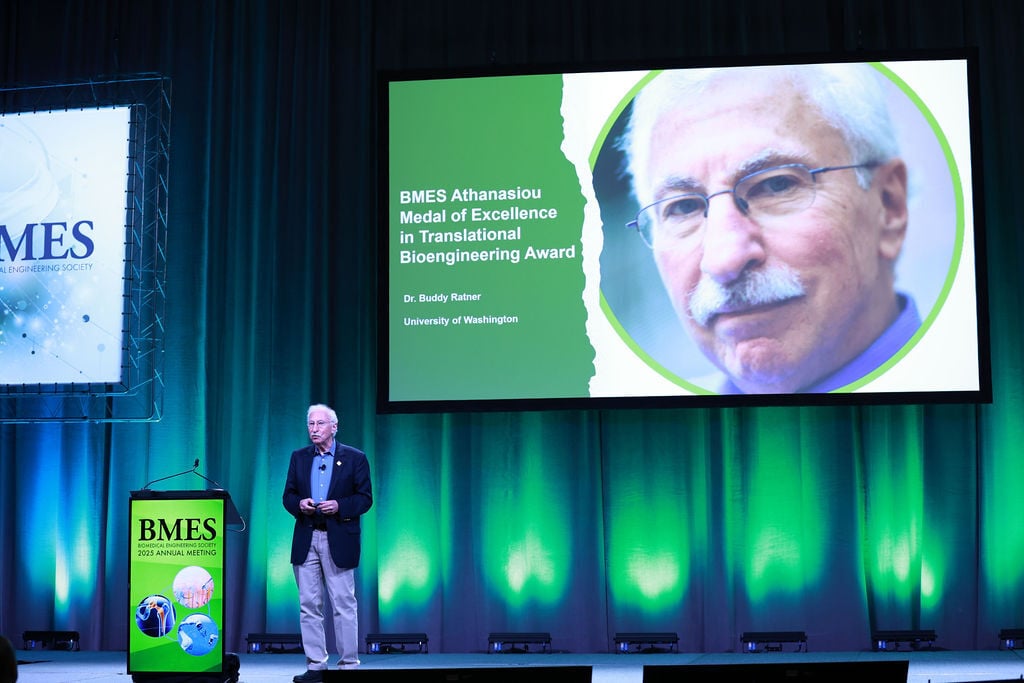
For Buddy Ratner, BMES Member and Professor of Bioengineering and Chemical Engineering at the University of Washington, translational bioengineering...

Two new Editors-in-Chief were selected for two prestigious Society journals: Keefe Manning, was named the new Editor-in-Chief of the Cardiovascular...

Greetings everyone!

Pritzker Distinguished Lecture: Mice, or Microfluidics? Humanizing Biomedical Research with “NAMs”
.jpg)
This is the fifth in a series of articles highlighting some of the technologies, processes and keynote plenary sessions presented at the 2024 Annual...